Start your payer engines
Trusted core administration and claims management engines
For the past 20 years, PLEXIS has honed our understanding of payer’s needs with our core administration & claims management solutions, and we’ve gone the extra mile with extensible business apps, our powerful Passport connectivity services, and a host of best-in-class professional services.
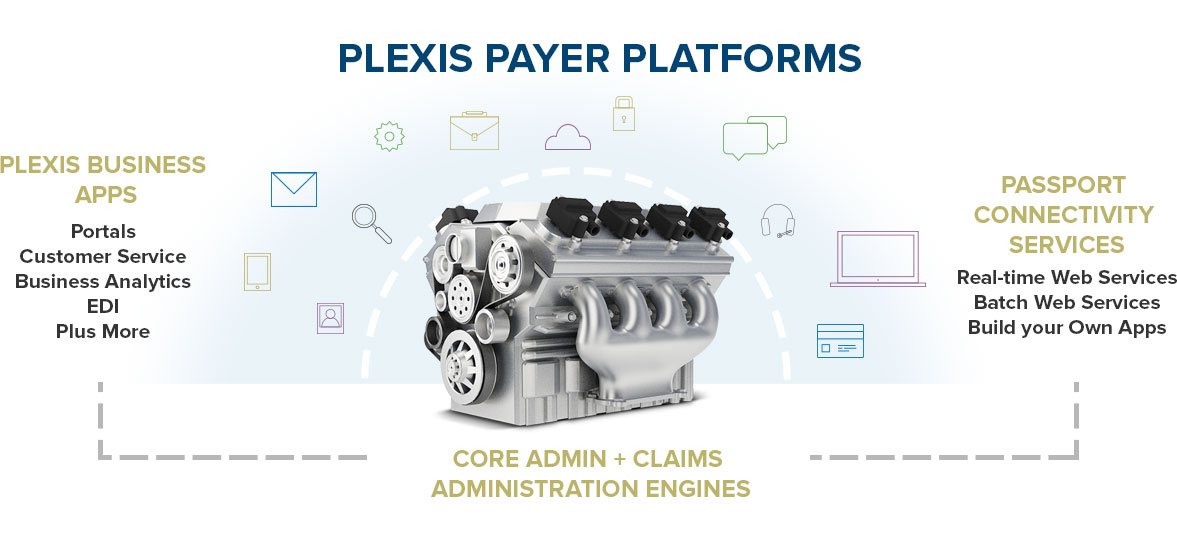
PLEXIS platforms are first and foremost trusted, time-tested core administration (benefit administration) and claims management engines. We empower domestic and international payer success through the solid technological foundation of our SQL-based platforms.
Easy to configure, agile enough to address demanding business needs, and flexible enough to capitalize on new growth opportunities, PLEXIS payer platforms deliver:
- Claims management, including claim auto-adjudication
- Benefit administration
- Robust member and eligibility management
- Premium billing administration
- Real-time claim editing
- Mass claim re-adjudication
- Intelligent alerts and reporting
- Provider administration/referrals and authorizations
- Capitation capabilities
- Easy-to-manage multi-level security
- Configurable add-ons such as external Medicare grouper and pricer routines
- Reference data loaders that automatically load procedure/diagnosis codes, UB04, NCCI data, etc.
See additional benefits of the most trusted core administration and claims management engines on the market:
- Process claims on a familiar Windows interface with hot keys.
- Save time managing membership and eligibility, including individuals who are dually eligible for Medicare and Medicaid.
- Meet cost containment objectives by investing in affordable core administrative processing technology for the greatest ROI.
- Automate complex benefit calculations and drive high auto-adjudication rates with PLEXIS’ rules-based engine.
- Simplify regulatory compliance with HIPAA-ready EDI (Electronic Data Interchange), supporting ICD-10, CMS 1500, and UB04.
- Conduct Encounter Reporting in compliance with CMS and state Medicaid protocols.
- Automation of claim late payment penalty and interest calculation.
- Stay in control of the information that various users are authorized to view with PLEXIS’ smart portal solution.
- A full library of standard reports available for use and custom modification.
- Send automated, intelligent alerts to a variety of user-defined media devices including a cell phone or pager using Business Activity Monitoring (BAM) via PLEXIS Alerts™
- Customize result/EOB codes and control their action (deny/pend/approve).
- Proactively implement changes before they take effect using effective from and through dates.
- Generate and manage AP and AR transactions automatically or manually.
- Drive outcomes with an agile, dependable software solution based on flexible configuration capabilities.
- Invest in technology with the assurance of proven reusability to ensure success throughout ongoing changes in healthcare policy and technology.

